 Stress incontinence or SI refers to when some activity like sneezing or coughing leads to a small quantity of urine leaking from the urethra, the tube which urine passes through. SI is the type of incontinence most commonly suffered by women, particularly older women. Women who have gone through childbirth have a higher chance.
Stress incontinence or SI refers to when some activity like sneezing or coughing leads to a small quantity of urine leaking from the urethra, the tube which urine passes through. SI is the type of incontinence most commonly suffered by women, particularly older women. Women who have gone through childbirth have a higher chance.
Facts About Stress Incontinence
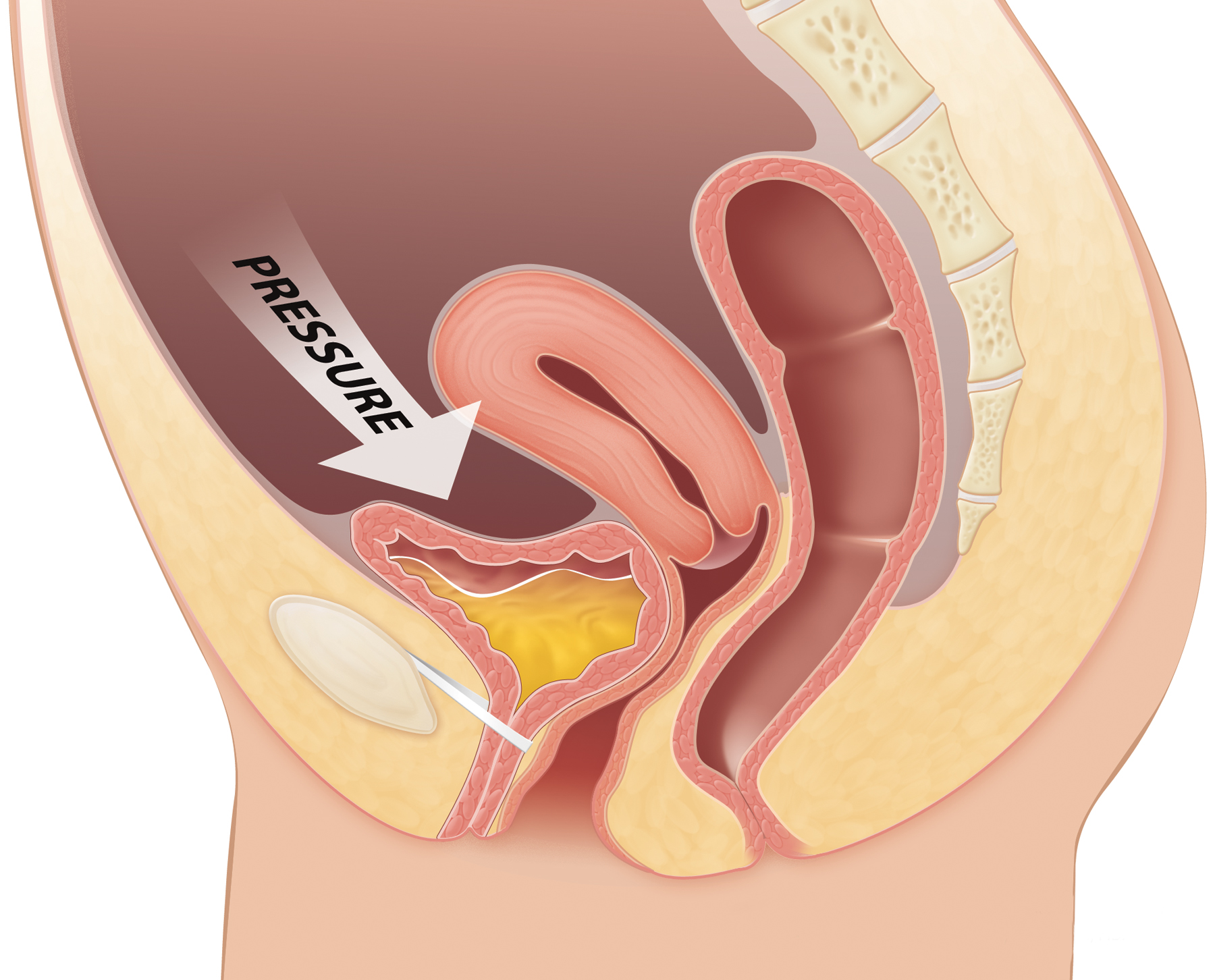
While urinary incontinence is unintentionally losing urine, stress incontinence occurs due to some type of physical activity or movement which puts pressure/stress on the bladder. Examples of activities include heavy lifting, running, sneezing or coughing.
Different from urge incontinence, stress incontinence involves unintentionally losing urine for the contracting of bladder muscles, which is typically associated with feeling urgent. It is actually the most common type of urinary incontinence and around three million women just within the UK experience regular incontinence. This issue becomes more common among older women and for those over 40 years old.
Experts believe that this number of people affected by stress incontinence is actually lower than the actual number, as many people feel embarrassed and don't tell their doctors. Some may think it simply can't be treated or is part of aging. The reality, however, is that many cases can be improved significantly or completely cured.
What Causes Stress Incontinence?
Many different things can lead to stress incontinence. It can, for example, be due to weak pelvic floor muscles or the weak sphincter muscle at the bladder's neck. Any issue with the way the sphincter muscle functions (opening and closing) may also lead to stress incontinence. Other possible factors include chronic coughing, obesity or smoking.
In many cases, particularly for women, stress incontinence is due to physical changes within the body, including:
- Weakened muscles surrounding the bladder
- Issues with the bladder's muscles and the urethra
- Menstruation
- Surgery
- Menopause
- Pregnancy and/or childbirth
When stress incontinence occurs, pelvic muscles may weaken. This in turn can lead to the bladder dropping so that the urethra cannot completely close, leading to urine leakage.
What Are the Symptoms?
The main symptom of stress incontinence is urine leakage during certain activities. Some of the activities that can frequently trigger this leakage include:
- Having sex
- Exercising
- Lifting something heavy
- Getting out of a vehicle or car
- Standing up
- Laughing
- Sneezing
- Coughing
Not everyone with stress incontinence will have leakage each time they perform the specific triggering action. Despite this, any activity that increases pressure on the area will increase the chances of accidentally losing urine and this is especially true in situations when the bladder is full.
How to Treat Stress Incontinence
1. Behavior Therapies
These therapies can help reduce stress incontinence episodes. Your doctor may suggest some of the following treatments:
- Exercises for the pelvic floor muscles: Doing kegel exercises will strengthen the pelvic floor muscles as well as the urinary sphincter. Your physical therapist or doctor can help you correctly do these exercises and the effectiveness of this treatment depends on how regularly you perform the exercises.
- Consuming fluids: In some cases, your doctor will suggest that you time your fluid consumption or limit it throughout the day. On a related note, he may also recommend avoiding alcoholic or caffeinated beverages until you can tell how the dietary irritants affect your bladder.
- Lifestyle changes: Many healthy lifestyle changes, such as treating chronic coughs, losing excess weight, and quitting smoking can improve symptoms and reduce your risk of stress incontinence.
- Scheduling toilet breaks: In cases of mixed incontinence, your doctor may suggest creating a toileting schedule, known as bladder retraining. By voiding your bladder more frequently, you can reduce the severity or number of incontinence episodes.
2. Devices
There are specific devices which have been designed for women and can help you control stress incontinence. These include:
- Vaginal pessary: This specialized incontinence pessary is fit and then your doctor or nurse places it. It is in a ring shape and has two bumps which sit on the two sides of your urethra. This device will support the base of the bladder, preventing urinary leaking while participating in activities. This is especially useful in cases of a prolapsed or dropped bladder. It is a good option for those who do not want surgery. Pessaries do require regular removal and cleaning and are frequently used in those with pelvic organ prolapse.
- Urethral inserts: Urethral inserts are disposable devices that resemble tampons and are inserted into your urethra. They form a barrier which prevents leakage. Although you can wear a urethral insert during the whole day, they are typically used for preventing incontinence when performing a specific activity. These are only used in rare cases, but shouldn't be worn for the entire day.
3. Surgery
Surgical interventions will help improve the sphincter's closure or support the neck of the bladder. Some of the surgical options include the following:
- Injectable bulking agents: Your doctor may inject synthetic gels or polysaccharides into the tissues surrounding the urethra's upper area. These materials help to bulk up this area, helping the sphincter close more easily. This intervention is not very invasive and as such, it is frequently considered before other surgeries. Despite this, most people need multiple injections, so this is not a permanent solution.
- Retropubic colposuspension: This procedure is done either via an abdominal incision or laparoscopically and it relies on attaching sutures to the bone or ligaments to help support and lift tissues close to the bladder neck as well as the upper area of the urethra. This procedure is frequently combined with others as a way to treat women with stress incontinence as well as a prolapsed (dropped) bladder.
- Sling procedure: The sling procedure is the most common surgical procedure for women who have stress urinary incontinence. The surgeon creates a hammock or slink to support the urethra using the patient's own tissue, synthetic mesh, or donor or animal tissue. This procedure also works in men who have sphincteric leakage and the mesh sling can help ease symptoms in men related to stress incontinence.
- Inflatable artificial sphincter: This involves implanting a surgical device and is mostly used for treating men, although it is appropriate for some women. The cuff fits around the urethra's upper area and takes over the sphincter's function. Tubes then connect this cuff with a balloon located in the pelvic region which regulates pressure as well as to a pump in the scrotum that is manually operated. In the rare cases that women receive the implant, the pump will be in the labia.
4. Home and Lifestyle Remedies
The following healthy lifestyle practices can help as well:
- Lose extra weight: If your BMI is higher than 25, then by losing excess weight, you can reduce the pressure on the pelvic floor muscles and bladder. Even moderate weight loss can help stress incontinence.
- Eat more fber: In cases where chronic constipation worsens the urinary incontinence, eating more fiber can keep the bowel movements regular and soft, helping to lower the strain on the pelvic floor muscles.
- Avoid bladder irritants: Those with mixed incontinence should avoid foods and beverages which can irritate their bladder. Coffee and tea tend to be bladder irritants for most people.
- Don't smoke: Smoking may give you a chronic cough which aggravates the stress incontinence. It also decreases your capacity for carrying oxygen, which can increase the chances of your bladder being overactive.